Jho Institute for Minimally Invasive Neurosurgery Department of Neuroendoscopy
Home | About Dr. Jho | Overview | Table of contents | Patient Registration Form | Directions, Contact & Hotel Information
Spine Diseases
Brain Diseases
Brain Tumor, Skull Base Tumor Surgery: Dr. Jho's Minimally Invasive Skullbase Surgery, Brain Tumor Surgery
Dr. Jho's Minimally Invasive Skull Base Surgery
Dr. Jho's Endoscopic Skull Base Surgery Through a Nostril: Minimally Invasive Skull Base Brain Tumor Surgery Without A Skin Incision
Professor & Chair, Department of Neuroendoscopy
Jho Institute for Minimally Invasive Neurosurgery
 Dr. Jho has developed minimally invasive endoscopic skull base surgery via a natural nostril for skull base tumors located at the midline (from the anterior frontal region to the distal clival area). The operation is performed through a nostril without any skin incisions. The tumor is removed with specially designed surgical instruments under endoscopic visualization.
Dr. Jho has developed minimally invasive endoscopic skull base surgery via a natural nostril for skull base tumors located at the midline (from the anterior frontal region to the distal clival area). The operation is performed through a nostril without any skin incisions. The tumor is removed with specially designed surgical instruments under endoscopic visualization.1. Endoscopic endonasal removal of the anterior skull base meningiomas via a nostril (without a skin incision)
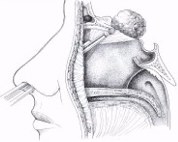
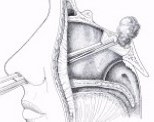
Figure 1. This schematic drawing demonstrates how anterior skull base meningiomas are removed via a nostril without any skin incisions. A 4-mm endoscope is inserted towards the base of the tumor at the skull base through a nostril. Surgical instruments are inserted next to the endoscope through the same nostril. The tumor is removed and the skull base is reconstructed. The patient's hospital stay is usually overnight.
A:  B:
B: 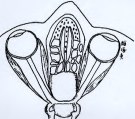
 B:
B: 
Figure 2. These schematic drawings demonstrate the area of surgical access gained by this endoscopic endonasal approach via a nostril to the anterior cranial fossa.
A:  B:
B: 
 B:
B: 
Figure 3. Intraoperative photographs show delivery of the tumor (A), the optic chiasm, pituitary stalk and anterior cerebral arteries after complete tumor removal (B).
2. Endoscopic endonasal removal of the clival or the posterior cranial fossa tumors via a nostril (without a skin incision)
A: B:
B: C:
C: 
 B:
B: C:
C: 
D:  E:
E: 
 E:
E: 
Figure 1. A schematic drawing displays endoscopic access to the clivus and posterior fossa through a nostril without a skin incision (A). The clivus can be approachable from the sella to the foramen magnum (B). The surgeon's endoscopic frontal view of the clivus is demonstrated (C). View under a 30-degree endoscope shows a tumor encasing the distal basilar artery and its branches. The posterior cerebral arteries (P) are visible (D). View under a 70-degree-lens endoscope after tumor removal shows the base of the brain with the superior cerebellar arteries (S), the bilateral posterior cerebral arteries (P), the posterior communicating arteries (Pc), the bilateral mammillary bodies (M), and the bilateral oculomotor nerves (III) (E).
A: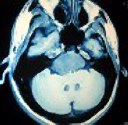 B:
B: C:
C: D:
D:
 B:
B: C:
C: D:
D:
Figure 2: MR scans, axial (A) and sagittal views (B), show a large chordoma in the clivus and posterior cranial fossa preoperatively. The tumor was totally removed with an endoscope through a nostril. The patient's hospital stay was overnight. Postoperative MR scans, axial (C) and sagittal views (D), demonstrate complete removal of the tumor. However, the tumor removal site was treated with gamma knife radiosurgery due to of the malignant nature of tumor.
3. Endoscopic endonasal removal of tumors at the cavernous sinus, optic nerve, sella, suprasellar region and pterygopalatine fossa via a nostril (without a skin incision)
Tumors involving the cavernous sinus, sella, suprasellar region, optic nerve, and pterygopalatine fossa can be removed through a nostril without a skin incision.
A: A:
A:  B:
B: 
 A:
A:  B:
B: 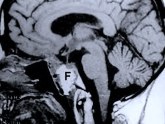
Figure 1. A schematic drawing demonstrates an endoscopic surgical approach to the sella, suprasellar region, cavernous sinus, optic nerve and pterygopalatine fossa area (A). A preoperative MR scan, sagittal view, shows a recurrent malignant pituitary tumor (T) (B). This postoperative MR scan demonstrates tumor removal and fat graft placement (F) at the tumor removal site (C).
A: 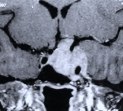 B:
B: 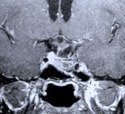
 B:
B: 
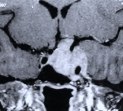
Figure 2. An MR scan, coronal view (A), shows a recurrent pituitary tumor involving the left cavernous sinus in another patient. The patient had undergone two previous transsphenoidal surgeries by another surgeon. The patient then underwent an endoscopic endonasal surgery for the recurrent cavernous sinus pituitary tumor. A postoperative MR scan, coronal view (B), shows complete tumor removal from the left cavernous sinus and anatomical preservation of the pituitary stalk and gland.
Facts About This Surgery
Discussion
After increased experience with endoscopic resections of pituitary tumors, it was noted that this technique could be applied to tumors of the skull base. Skull base tumors such as chordomas, epidermoid tumors, meningiomas, craniopharyngiomas, germinomas, etc. can now be removed through a patient's nostril when anatomically applicable. This new technique, utilizing endoscopic visualization, avoids extensive face-disfiguring surgical exposure and naturally facilitates quick postoperative recovery. Patients are often able to leave the hospital the day after their surgery.
The condition of cerebrospinal fluid leakage (CSF leak) occurring spontaneously through the nose or developing after some types of sinus surgery can also be easily repaired with this endoscopic technique.
References
Dr. Jho's Minimally Invasive Transcranial Skull Base surgery
Jho Institute for Minimally Invasive Neurosurgery
1. Dr. Jho's "Band-aid" Nose-Bridge Skull Base Surgery: Glabellar Approach: A Minimally Invasive Skull Base Brain Tumor Operation
Dr. Jho has develped minimally invasive midline anterior cranial base surgery via a small skin incision at the nasal bridge. When an endoscope is adopted, this small incision skull base surgery provides wide visualization at the anterior cranial base for tumor removal. This "Band-aid" skull base brain surgery has been applied for midline skull base tumors such as meningiomas, nasopharyngeal carcinomas, craniopharyngiomas, olfactory neuroblastomas and other skull base tumors. Postoperative incisions are so small as to be covered only by a "Band-Aid" type dressing, hence the name "Band-Aid" skull base brain surgery.
A:  B:
B:  C:
C: 
 B:
B:  C:
C: 
Figure 1. A preoperative MR scan, coronal view (A), reveals a large meningioma. An intraoperative picture (B) shows the optic chiasm and bilateral optic nerves after complete tumor removal. Postoperative MR scan (C) confirms total tumor removal through a small skin incision at the nose-bridge.
A:  B:
B:  C:
C:  D:
D: 
 B:
B:  C:
C:  D:
D: 
Figure 2. Preoperative MR scans, axial (A) and sagittal (B) view, disclose a large anterior fossa meningioma in an elderly woman. The tumor was totally removed under an endoscope via a 2-cm skin incision at the nose bridge. Postoperative MR scans, coronal (C) and sagittal (D) view, confirm complete removal of the tumor via a glabellar approach. A postoperative MR scan, sagittal view (D), shows an abdominal fat graft (white) placed in the ethmoid and frontal sinus in order to prevent the possible postoperative cerebrospinal fluid leakage.
A:  B:
B: 
 B:
B: 
Figure 3. Pictures (A) demonstrate the line for the skin incision (Top), postoperative bandage (Middle), and the healed incision (Bottom). Preoperative visual field testing results (B: Top) display significant visual field defects portrayed by blackened areas (almost blind bilaterally). After total removal of an anterior skull base meningioma via a glabellar approach, postoperative visual field results (B: Bottom) on the same patient display significant improvement in visual fields.
A:  B:
B:  C:
C: 
 B:
B:  C:
C: 
Figure 4. Evolution of a glabellar skin incision. When an endoscope is utilized instead of the operating microscope a much smaller incision can be used. The photograph shows a postoperative bandage placed over a skin incision (A). The skin incision at the nose bridge as seen morning after surgery (B). Healed glabellar skin incision seen six weeks following surgery (C).
Facts About This Surgery
Discussion
In order to minimize the size of skin and bone openings that are commonly used in conventional skull base (also called cranial base) procedures, a surgical approach has been developed that allows the surgeon a direct shortcut type of approach to tumors of the anterior skull base. Called the glabellar approach (or "Band-Aid"), it utilizes a three- to four-cm incision above the nose and between the eyes, the area known anatomically as the glabella. It is a modification of the frequently used frontal approach but does not incorporate the use of brain retractors, minimizing the potential for brain injury.
Positive reports have been received concerning the cosmetic outcome of the incision as well. Great effort was taken to develop a "straight-line-to-the-problem" type of surgical approach that also focuses on preservation of surrounding anatomical structures. This approach is analogous to the efforts of those who restore great works of art, bringing back the brilliance of the original work without disturbing the original content. Care is taken in the glabellar approach to accomplish tumor removal with minimal disruption of surrounding structures.
Definitions
glabellar - referring to the anatomical region at the top of the nose between the eyes.
Reference
2. Dr. Jho's Minimally Invasive Operation For Meningiomas, Craniopharyngiomas, And Cerebral Aneurysms: "Band-aid" Eyebrow Incision Skull Base Surgery: Orbital Roof (Orbitofrontal) Craniotomy
Dr. Jho has developed minimally invasive transcranial skull base surgery via a small eyebrow incision. This "Band-aid" brain surgery, orbitofrontal skull base surgery via an eyebrow incision, has been used for meningiomas, craniopharyngiomas, parasellar tumors and cerebral aneurysms.
A: B:
B: C:
C: D:
D:
 B:
B: C:
C: D:
D:
Figure 1. An MR scan, sagittal view, shows a large tumor (teratoma) beneath the brain preoperatively (A). An MR scan, sagittal view, demonstrates complete tumor removal postoperatively (B). A picture depicts a line drawn for the skin incision in the operating room that follows the contour of the eyebrow (C). The healing incisional line soon after surgery (D).
A: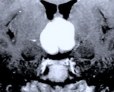 B:
B: C:
C: D:
D: E:
E:
 B:
B: C:
C: D:
D: E:
E:
Figure 2. MR scans, axial view (A) and sagittal view (B) display a large craniopharyngioma in the third ventricle. Postoperative MR scans, coronal (C) and sagittal views (D), confirm complete tumor removal. A patient following an orbitofrontal craniotomy via an eyebrow incision (E). A small bandge along the contour of the right eyebrow can be seen.
A:  B:
B:  C:
C:  D:
D: 
 B:
B:  C:
C:  D:
D: 
Figure 3. Preoperative MR scan, axial view (A), shows a meningioma (a gray round shadow at the upper center) with severe surrounding brain edema (white). Two photographs (B) of a postoperative patient show a covered eyebrow incision in the recovery room and a healed incision at 6 weeks after surgery. Postoperative MR scans, sagittal (C) and axial (D) views, confirm complete tumor removal.
A:  B:
B: 
 B:
B: 
Figure 4. An intraoperative photograph (A) provides a clear image of the bilateral optic nerves and chiasm with tumor (red) adhered in a patient with a sellar meningioma. Another intraoperative photograph (B) shows the optic nerve system after complete removal of the tumor via an eyebrow incision craniotomy.
A:  B:
B:  C:
C: 
 B:
B:  C:
C: 
Figure 5. A preoperative MR scan, coronal view, shows a craniopharyngioma (white) (A). A postoperative MR scan, coronal view, displays complete removal of the tumor via an orbitofrontal craniectomy (B). Surgery was performed under the endoscopic visualization. The optic nerve system and anterior cerebral arteries are well visualized after total tumor removal (C).
Facts About This Surgery
Discussion
This minimally invasive approach to the skull base provides the surgeon with exposure to the anterior fossa and parasellar region. Anatomically, this is the front portion of the skull base behind the nose and eyes, and includes the area near the pituitary gland. It is done through a hole in the skull about an inch long and utilizes a skin incision above the eyebrow that is about three- to four-cm long. Positive patient input has been received concerning the cosmetic outcome of the healed incisions.
Not only does this procedure provide acceptable cosmetic outcome, it provides effective and direct exposure for tumor removal (as well as for clipping of cerebral aneurysms). The idea behind this procedure is analogous to the idea behind mining tunnels that were once constructed by coal miners. The coal miners had to ensure that the tunnels were wide enough to permit the motion of their tools (picks and shovels). They had the difficult task of creating a tunnel small enough so as to not weaken the ground above but large enough to permit work to take place.
This surgery, by utilizing the natural anatomical spaces and cavities of the brain, provides the surgeon with an ample working space that does not endanger the surrounding structures. Neither outcome or exposure is sacrificed in providing patients with alternative surgical techniques that approach a surgically challenging anatomical area.
Definitions
craniotomy - an operation producing an opening in the cranium.
Reference
3. Dr. Jho's Minimally Invasive Surgery For Brain Tumors And Cerebral Aneurysms:
"Band-aid" Superolateral Orbital Craniotomy:
Dr. Jho has developed minimally invasive skull base surgery ("Band-aid" skull base brain surgery) via a small lateral eyebrow incision for meningioma, epidermoid, craniopharyngioma, parasellar tumors, and cerebral aneurysms.
A: B:
B: C:
C: D:
D:
 B:
B: C:
C: D:
D:
E: F:
F:
 F:
F:
Figure 1. Preoperative MR scans, coronal (A) and sagittal views (B), reveal a tuberculum sellar meningioma which caused a visual disorder in this patient. Postoperative MR scan, coronal (C) and sagittal views (D), demonstrate complete removal of the tumor via an eyebrow approach. A photograph demonstrates the postoperative bandage after total resection of the tumor (E). Visual field test depicts a visual field defect, seen as the darkened area, which is caused by tumor compression on optic nerve system (A in F). After tumor removal, the visual field recovered (B in F).
A:  B:
B:  C:
C: 
 B:
B:  C:
C: 
Figure 2. A preoperative cerebral arteriogram (A) shows a basilar tip aneurysm. A postoperative arteriogram, after aneurysm clipping via a superolateral orbital craniotomy, confirms successful clipping (B). A patient with a healed superolateral orbital craniotomy incision line (C) (arrows).
Facts About This Surgery
Discussion
Utilizing a small hole in the skull above and to the side of the eyebrow, this minimally invasive skull base procedure provides a direct "shortcut" approach to tumors and aneurysms. Nicknamed Band-aid surgery because a Band-Aid type dressing is all that is required to cover the postoperative incision, this surgery does not sacrifice exposure for the surgeon while providing the benefits of being less invasive. Tumors and aneurysms located laterally at the anterior skull base are reached through a two-inch skin incision and a small bone hole called a craniotomy. It is referred to as a superolateral craniotomy because the approach is above the eye and slightly to the side. Brain retractors are not used, which reduces the risk of brain injury. Positive feedback has been received concerning the cosmetic healing of incisions.
Definitions
orbital - refers to the bony cavity in the skull that contains the eyeball.
Reference
4. Dr. Jho's "Band-aid" Temple-Incision Skull Base Surgery: Subtemporal Approach: Minimally Invasive Brain Tumor Surgery
Dr. Jho uses this technique of minimally invasive middle cranial fossa skull base surgery ("Band-aid" skull base brain surgery) for cavernous sinus tumors, tentorial meningiomas, cholesterol granulomas, trigeminal neurilemmomas, petroclival meningiomas, and cerebral aneurysms.
A: B:
B: C:
C: D:
D: E:
E:
 B:
B: C:
C: D:
D: E:
E:
Figure 1. Preoperative MR scans, axial (A) and coronal views (B), reveal a large meningioma involving the cavernous sinus and tentorium. A patient wears a postoperative bandage after total tumor removal via a subtemporal approach (C). The patient did well following surgery and only experienced some residual left-sided facial numbness. Postoperative MR scans, axial (D) and coronal (E) views, confirm complete tumor removal.
Facts About This Surgery
Discussion
The traditional approach of a subtemporal craniotomy has been modified. Now tumors and vascular lesions of the middle cranial fossa skull base, cavernous sinus, petrous bone, and upper posterior cranial fossa can be reached through a smaller skull hole and through a smaller skin incision. A two-inch skin incision and a compact, strategically placed skull hole is made at the temple for access to the middle fossa, cavernous sinus, and tentorial regions. The incision is covered by a "Band-Aid" after surgery and patients generally only need to stay in the hospital for two or three days. This surgery is a minimally invasive alternative for both tumors and vascular lesions.
5. Dr. Jho's "Band-Aid" Retromastoid Craniotomy: Minimally Invasive Brain Surgery
Dr. Jho uses a retromastoid approach as minimally invasive Band-Aid posterior fossa surgery for acoustic neuromas, meningiomas, epidermoids, trigeminal neuromas, glossopharyngeal or vagal neuromas, glomus jugulare tumors, trigeminal neuralgia, hemifacial spasm, vertigo, tinnitus, glossopharyngeal neuralgia, and vertebrobasilar aneurysms. Brain retractors are not used in order to avoid any brain damage by metallic retraction of the brain.
A:  B:
B: 
 B:
B: 
Figure 1. A preoperative MR scan, axial view (A), reveals an acoustic neuroma. An immediately postoperative axial CT scan (B) demonstrates complete removal of the acoustic tumor accomplished via a retromastoid craniectomy approach.
A:  B:
B: 
 B:
B: 
Figure 2. An intraoperative photograph shows tumor removal at the internal auditory canal during a retromastoid craniectomy approach (A). This intraoperative photograph demonstrates complete removal of an acoustic neuroma and the preserved facial and hearing nerves (B).
A:  B:
B: 
 B:
B: 
Figure 3. Immediate postoperative patient photographs demonstrate normal facial nerve function following retromastoid craniectomy for acoustic tumor removal. The patient's hearing was also well preserved.
Facts About This Surgery
Discussion
This technique involves a small hole in the skull through a short skin incision. Retromastoid refers to the region behind the ear. This technique is ideal for removal of tumors such as acoustic neuromas, trigeminal neuromas, glossopharyngeal or vagal neuromas, glomus jugulare chemodectomas, and other tumors located at the cerebellopontine angle. Combining delicate microsurgical skills with sophisticated electrophysiologic monitoring makes the chance of preserving hearing and facial nerve function very high in acoustic neuroma surgery. This approach is also utilized for surgical treatment of vertebrobasilar aneurysms and cranial nerve problems such as trigeminal neuralgia (tic douloureux), and hemifacial spasm. The surgical incision requires only a small dressing and patients often only need to stay in the hospital for three to five days.
6. Dr Jho's Lateral Approach to the Craniocervical Junction: Minimally Invasive Skull Base Surgery For Brain Tumors And Cerebral Aneurysms
Dr. Jho uses a minimally invasive skull base approach via a small straight skin incision at the side of the upper neck, for tumors at the craniocervical junction. A bone window is made at the strategic access point to the tumors or aneurysms without unnecessary dissection or destruction of the anatomical structures. These modified techniques help to speed up patient's postoperative recovery with less discomfort, in addition to effectively eradicating the lesion.
A: B:
B: C:
C: D:
D:
 B:
B: C:
C: D:
D:
E:  F:
F: G:
G:
 F:
F: G:
G: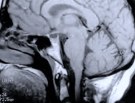
Figure 1. Preoperative MR scans, axial (A) and sagittal (B) views, reveal a meningioma that is severely compressing the medulla at the craniocervical junction. Intraoperative photographs demonstrate a large meningioma (C) and a frontal view of the cervicomedullary junction after complete tumor removal (D). A postoperative patient photograph (E) shows the small skin incision utilized in this posterolateral approach to the craniocervical junction. Postoperative MR scans, axial (F) and sagittal (G) views, confirm complete removal of the tumor.
Practice Manager: Robin A. Coret
Tel : (412) 359-6110
Fax : (412) 359-8339
Address : JHO Institute for Minimally Invasive Neurosurgery
Department of Neuroendoscopy
Sixth Floor, South Tower
Allegheny General Hospital
320 East North Avenue
Pittsburgh, PA 15212-4772
Copyright 2002-2032