Jho Institute for Minimally Invasive Neurosurgery Department of Neuroendoscopy
Spine Diseases
Brain Diseases
Lumbar Stenosis: Dr. Jho's No-fusion Endoscopic Decompression Lumbar Stenosis Surgery
Dr. Jho's Minimally Invasive Lumbar Stenosis Surgery: Endoscopic Decompression via Microforaminotomy for Lumbar Stenosis
Professor & Chair, Department of Neuroendoscopy
Jho Institute for Minimally Invasive Neurosurgery
Dr. Jho developed a minimally invasive endoscopic decompression surgery for lumbar stenosis. Surgery involves a small skin incision at the lumbar region, the placement of a small trocar, endoscopic foraminotomy, and widening of the narrowed spinal canal through a endoscopic foraminotomy hole. Unlike the conventional laminectomy surgery, most posterior spinal structures are well preserved in order to minimize postoperative weakening of the spine. Multiple level surgery can be performed if required.
Figure 1. Dr. Jho's endoscopic decompression

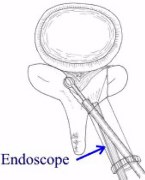
A 1.5 cm trocar is placed via a 2-cm skin incision at the lumbar area (upper photograph). A small foraminotomy hole is made at a stenotic segment of the lumbar spine. Through this small foraminotomy hole, the stenotic spinal canal is enlarged bilaterally (a schematic drawing). The operation can be performed at multiple levels. This anatomy-preserving surgery minimizes surgical impact to the spine. Unlike conventional laminectomy surgery, the spinal integrity (including the anatomy and function) is preserved with this endoscopic surgery. This functional lumbar stenosis surgery does not require bone fusion or metal plate implantation. Thus, surgical recovery is fast. In particular, the minimally invasiveness of this surgery enables elderly patients to ambulate soon after surgery.
A:  B:
B: C:
C: D:
D:
 B:
B: C:
C: D:
D:
Figure 2. MR scans, axial (A) and sagittal (B) views, in an elderly patient with neurogenic claudication reveal stenosis at L3-4 and L4-5 preoperatively. The patient underwent endoscopic decompression at both levels. Postoperative MR scans, axial (C) and sagittal (D) views, demonstrate wide decompression bilaterally at the spinal canal.
Pathoanatomy of lumbar stenosis
Lumbar stenosis is a condition in which the spinal canal (where spinal nerves pass) is narrowed and causes symptoms by compression of the spinal nerves. It can be subdivided into congenital stenosis and acquired stenosis.
Congenital stenosis can occur with particular diseases; however, it can also occur in the general population (who do not have any particular disease conditions). Some people are born with a relatively narrow spinal canal. They may remain asymptomatic until a minor degenerative process causes further narrowing of the spinal canal.
Acquired stenosis is the second and most common type, which is due to degenerative changes. With degeneration of the disc, the height of the disc decreases while the width of the disc increases, accompanied by protrusion of the disc and bone spur formation at the edge of the vertebrae. The facet joints, which are the two sliding articular joints at the posterior portion of the spinal motion unit, develop arthritic changes that consist of bone spur formation and overgrowth of the joint capsule. Narrowing of the spinal canal (lumbar stenosis) occurs with the combination of changes in the disc and facet joints.
Symptoms of lumbar stenosis
Most patients complain of low back pain as their main symptom. However, there is usually no direct correlation between the degree of spondylotic changes and the degree of low back pain. The narrowing of the spinal canal can occur diffusely or focally. Focal stenosis can cause symptoms related to the nerve root that is compressed. It can cause severe sharp pain in the leg, or burning and numbing sensations in the leg. Diffuse stenosis can cause burning and numbing sensations or pain in the leg, difficulty in walking, weakness in the legs, muscle loss, and difficulty in bowel and bladder control. Patients develop those symptoms when they try to walk some distance (neurogenic claudication). When they sit down or bend forwards for a few minutes, they will note improvement of their symptoms. The symptoms improve in this position because their spinal canal opens up to some degree when the spine bends forward. Riding a bike is easier for them than walking because riding a bike keeps their lumbar spine bent forward. Pushing a supermarket cart with a leaning-forward posture is often easier for patients as well.
Treatments
Treatments consist of conservative treatments and surgical treatments. Conservative treatments include medications, physical therapy, chiropractic treatment, local blocks, epidural blocks, steroid treatment, etc. When conservative treatments do not improve their symptoms, surgical treatments may be required.
For focal stenosis, surgical treatment is directed to release of compression at the exact pathologic site. For diffuse stenosis, conventional surgical treatment is decompressive laminectomy. Dr. Jho developed endoscopic decompression surgery for focal stenosis as well as diffuse stenosis. Dr. Jho's endoscopic decompression for focal stenosis accomplishes release of compression by providing the compressed nerve with a wider passage route. Dr. Jho's endoscopic decompression of diffuse stenosis achieves widening of the narrowed spinal canal bilaterally through a small foraminotomy hole. By doing so, most bony anatomy is preserved (contrary to the conventional laminectomy technique). Dr. Jho's technique eliminates the use of bone fusion or metal implants that have been in common use by spine surgeons in recent years.
Facts About This Surgery
Discussion
Degenerative spondylotic spine disease, which causes break down of the vertebrae, narrows the spinal canal and can lead to symptoms of pain, numbness, tingling, weakness as well as difficulties in walking or urinating. An analogy of the disease process would be to picture a coal mine tunnel that has partially collapsed, making the passageway narrow in some areas. This condition is referred to as lumbar stenosis. Conventional surgical treatment involves removing large portions of bone (called lamina). A new procedure has been developed to achieve widening of the spinal canal while only making small holes in the bone, referred to as endoscopic foraminotomy. The advantage of this procedure is its ability to maintain the overall structural strength of the spine and to decrease postoperative discomfort. This is accomplished through a tiny incision and usually allows the patient to go home the following day.
Reference
Practice Manager: Robin A. Coret
Tel : (412) 359-6110
Fax : (412) 359-8339
Address : JHO Institute for Minimally Invasive Neurosurgery
Department of Neuroendoscopy
Sixth Floor, South Tower
Allegheny General Hospital
320 East North Avenue
Pittsburgh, PA 15212-4772
Copyright 2002-2032