Jho Institute for Minimally Invasive Neurosurgery Department of Neuroendoscopy
Home | About Dr. Jho | Overview | Table of contents | Patient Registration Form | Directions, Contact & Hotel Information
Spine Diseases
Brain Diseases
Cervical Disc Herniation: Dr. Jho's No-fusion Anterior Microforaminotomy Cervical Disc Herniation Surgery
Dr. Jho's Minimally Invasive, Disc Preserving, Functional Cervical Disc Surgery: Anterior Microforaminotomy
(Jho Procedure)
Professor & Chair, Department of Neuroendoscopy
Jho Institute for Minimally Invasive Neurosurgery
 Dr. Jho believes that spine surgery should be a minimally invasive, anatomy-maintaining and function-preserving treatment (it can be named "functional spine surgery"). Current conventional treatments such as bone fusion and metal plate-screw implantation in the spine are not anatomical, not physiological, and thus, not functional. On the other hand, the Jho procedure for cervical disc herniation achieves direct removal of the herniated disc or protruded bone spurs, while preserving the remaining normal disc and spine motion intact. It is performed through a small foraminotomy hole (5 mm) made at the side of the cervical spine via a small skin incision made at the anterior neck.
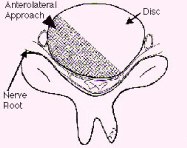
Dr. Jho believes that spine surgery should be a minimally invasive, anatomy-maintaining and function-preserving treatment (it can be named "functional spine surgery"). Current conventional treatments such as bone fusion and metal plate-screw implantation in the spine are not anatomical, not physiological, and thus, not functional. On the other hand, the Jho procedure for cervical disc herniation achieves direct removal of the herniated disc or protruded bone spurs, while preserving the remaining normal disc and spine motion intact. It is performed through a small foraminotomy hole (5 mm) made at the side of the cervical spine via a small skin incision made at the anterior neck.Figure 1: Summary of the "Jho procedure" for cervical disc herniation
A:  B:
B: 
 B:
B: 
Jho procedure for cervical disc herniation was developed in order to accomplish direct removal of the herniated disc or protruded bone spurs while preserving the remaining normal disc and spine motion intact. It is performed through a small foraminotomy hole (5 mm) made at the side of the cervical spine via a small skin incision made at the anterior neck. The square in the spine model (A) and the arrows in the postoperative roentgenogram (B) indicate a foraminotomy hole site at the C5-6. Herniated disc material or bone spurs are removed through this hole. Bone fusion is not necessary. Postoperatively, patients do not wear a cervical collar and will have normal neck motion immediately.
A:  B:
B: 
 B:
B: 
Figure 2 : A preoperative MR scan, axial view (A), shows nerve root compression by herniated disc material at C5-6 (arrow). A postoperative MR scan, axial view (B) displays a widened nerve root canal after disc removal via the Jho procedure.
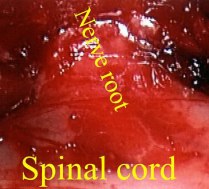
Figure 3: An intraoperative magnified picture shows the decompressed nerve root (long arrows) from its origin at the spinal cord (short arrows) to the exit site behind the vertebral artery. The microforaminotomy hole is approximately 5 mm in size.
A: B:
B: C:
C: D:
D: E:
E:
 B:
B: C:
C: D:
D: E:
E:
Figure 4. Postoperative MR scan and X-rays after Jho procedure at left C5-6.
A: A postoperative MR scan, sagittal view, depicts preservation of the remaining disc at C5-6 (arrow).
B: An oblique x-ray taken postoperatively reveals the widely opened neural foramen at the left C5-6 (arrows).
C: The opened nerve passage at the left C5-6 can be viewed in this anteroposterior view x-ray (arrows).
D, E: Postoperative flexion and extension dynamic x-rays demonstrate maintenance of the motion segment as well as spinal stability following left C5-6
microforaminotomy.
Dr. Jho's alternative minimally invasive cervical disc surgery
1. Percutaneous endoscopic anterior cervical discectomy
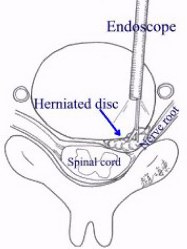
When the herniated disc is a soft fragment, the herniated disc fragment can be removed via a percutaneous endoscopic approach. Through a small skin incision at the anterior neck, a small trocar is placed at the anterior aspect of the cervical spine. A small trocar is advanced through the disc space towards the herniated disc. An endoscope is inserted through the trocar. Under direct endoscopic visualization, herniated disc fragments are excised. Unlike the Jho procedure described above, this surgical approach is made through the intervertebral disc space. Thus, the intervertebral disc is partially disrupted by the surgical procedure.
2. Posterior endoscopic foraminotomy
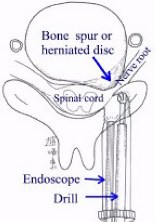
Posterior foraminotomy is a classic conventional treatment for cervical disc disease. In order to make this surgery minimally invasive, Dr. Jho has adopted the use of an endoscope instead of the operating microscope for this surgery. Through a small skin incision at the posterior neck, a small trocar is placed at the target area where the nerve is pinched. The nerve decompression is performed with an endoscopic foraminotomy. Unlike the Jho procedure described above, this operation does not eliminate the compressing bone spurs anterior to the nerve root, but provides extra room posteriorly for the compressed nerve root. However, this operation does not require bone fusion, thereby maintaining motion at the operated level. A schematic drawing demonstrates this posterior endoscopic foraminotomy (left), and an Intraoperative photo reveals the decompressed nerve root (right).
ANATOMY OF THE CERVICAL SPINE: The spine generally consists of columnar-shaped vertebral bones and discs in-between. The cervical spine refers to the spinal column in the neck region which consists of seven vertebrae. Intervertebral discs do not exist between the cranium and the first vertebra and between the first vertebra (called the atlas) and second vertebra (called the axis). Intervertebral discs are present between C2-3 (between the second and third vertebra), C3-4, C4-5, C5-6, C6-7 and C7-T1 (between the seventh cervical vertebra and the first thoracic vertebra). Because most bending motion in the cervical spine occurs at the C4-5, C5-6 and C6-7, disc displacement or disc herniation occurs most commonly at those levels. The intervertebral disc is composed of four elements: the nucleus pulposus at the very center, the annulus fibrosus as a thick envelope that contains the gelatinous nucleus pulposus at the center, the cartilaginous plate superiorly and inferiorly at the vertebral bone side, and the ligaments that surround the annulus fibrosus circumferentially.
TYPES OF CERVICAL DISC HERNIATION: Although the term "disc herniation or herniated nucleus pulposus (HNP)" has been commonly used for cervical disc disease, the displacement of the nucleus pulposus is not always the cause of cervical disc disease. Cervical disc herniation can be categorized into three different types: (1) a soft disc herniation that involves herniation of the nucleus pulposus through a tear at the annulus fibrosus, (2) a hard disc protrusion that is bone spur formation, or (3) a combination of both. When soft disc materials of the nucleus pulposus herniates out through a tear of the annulus fibrosus, it is called "soft disc herniation" because the herniated disc material is soft in its consistency. However, without a tear or defect at the annulus fibrosus, symptoms of cervical disc disease can still occur due to bone spurs (or overgrowth of bone spicules) developing over time at the edge of the vertebra which compresses the nerve root or spinal cord. This is called "hard disc herniation" because it is made of bony spurs. A combination of both conditions can occur as well.
CLINICAL SYMPTOMS: Symptoms can be categorized into three different groups. The first group of symptoms include neck pain, pain between wing bones, scapular pain, posterior head pain, difficulty in neck motion, and dizziness, especially when the neck is bent backward or turned to the side. These symptoms are thought to be produced by local compression of the ligaments and the surrounding anatomy. The second group of symptoms include pain along the shoulder, arm and hand, numbness in the hand and fingers, and weakness of the arm (radiculopathy). This second group of symptoms is produced by compression of the passing nerve root. The third group of symptoms includes numbness in the arms, torso and/or legs, difficulty in balance, gait disorder, clumsy spastic legs, and difficulty in bowel and bladder control (myelopathy). This third group of symptoms is caused by compression of the spinal cord.
TREATMENTS: Disc disease in the spine is one of the common problems that people experience. Treatments consist of conservative treatments and surgical treatments. Conservative treatments include physical therapy, chiropractic manipulation, nerve block, steroid treatment, pain medications, etc. When symptoms do not improve with conservative treatments, surgical treatments have to be considered. Current conventional surgical treatments fall into two different types: (1) anterior discectomy with bone fusion, and (2) posterior foraminotomy. Anterior discectomy and fusion will sacrifice the spinal motion at the herniated disc level. The posterior foraminotomy technique avoids bone fusion but often does not efficiently eliminate the herniated disc materials. In order to overcome drawbacks of the current conventional surgical treatments for cervical disc herniation, a new surgical treatment called ďanterior cervical microforaminotomy (Jho procedure)?/B> was developed by Dr. Jho.
Dr. Jhoís anterior microforaminotomy provides an effective elimination of the compressing herniated portion of the disc or bone spurs, while preserving the remaining disc between the vertebrae and maintaining spinal motion. Figure 2A demonstrates a herniated disc at the C5-6 in an axial view of an MR scan, and Figure 2B displays complete removal of the herniated disc material postoperatively. Figure 3 shows the nerve root and spinal cord after removal of the herniated disc material. Figure 4A reveals preservation of the intervertebral disc between C5 and C6 vertebra in a postoperative MR scan sagittal view. Figure 4B is a postoperative oblique x-ray demonstrating a left C5-6 anterior foraminotomy hole. Figure 4C shows a small bone opening site at the C5-6 level in order to enlarge the nerve foramen. Flexion and extension dynamic X-rays demonstrate good normal motion at the C5-6 postoperatively (Figure 4D).
Facts About the Jho Procedure for Cervical Disc Herniation
Discussion
The focus of this newly developed surgery centers on removal of the bony spur or disc material that is pressing on the nerve root causing "electric," "numbing," or "shooting" pains, that often start in the neck and travel into one or both arms. Through a small skin incision at the front of the neck, the source of the problem (the disc material or bony spur) can be clearly seen through a small hole made at the side of the intervertebral disc. Only the protruding disc material or bone spur is trimmed away, leaving the majority of disc material and bone undisturbed.
This is a less invasive method (which is able to preserve the neck joint or motion segment) than the conventional anterior discectomy procedure (which eventually leads to fusion of the bone). Patients are most often able to go home without neck braces on the day of surgery or the day following surgery, with noticeable relief from the nerve pain in their arms. Candidates for this surgery include patients who have herniated cervical discs or bony spurs pinching the nerve root causing neck pain and radiating pain to one or both arms, not relieved by at least three weeks of conservative treatment. This does not necessarily exclude patients who have undergone previous neck surgeries.
Definitions
foraminotomy - enlargement of an opening or passageway for a nerve.
myelopathy-pertaining to symptoms and signs caused by the spinal cord.
radicular pain - pertaining to pain caused by a nerve root.
References
Cervical Stenosis
Dr. Jho's Minimally Invasive Cervical Stenosis Surgery (The Jho procedure for cervical stenosis): Spinal Cord Decompression via Anterior Foraminotomy for Spondylotic Cervical Stenosis, or Ossified Posterior Longitudinal Ligament (OPLL)
Professor & Chair, Department of Neuroendoscopy
Jho Institute for Minimally Invasive Neurosurgery
In order to accomplish minimally invasive, efficient elimination of the compressive pathology to the spinal cord and to maintain the motion segment, the Jho procedure for Cervical Stenosis Surgery was developed. The compressing pathology is removed via a small microforaminotomy hole or holes made at the side of the cervical spine via a small incision made at the anterior neck (Figure 1). This operation does not require bone fusion or metal plate-screw implantation.
Cervical stenosis is a disease condition that narrows the spinal cord canal in the cervical spine and causes symptoms of spinal cord compression. Although similar to Cervical Disc Herniation in many ways, Cervical Stenosis involves a narrowing of the spinal canal that chokes the spinal cord rather than a focal protrusion of disc material that compresses a part of the spinal cord and/or nerve roots.
Cervical stenosis can be categorized into two different types: a congenital form and an acquired form. Although various congenital conditions may cause the narrowing of the spinal cord canal, it is also possible for normal people to have a relatively narrow spinal cord canal at birth. The acquired form of cervical stenosis is generally developed by wear-and-tear. In Cervical Stenosis, the intervertebral discs are protruded and bony spurs are built-up all along the edges of the vertebrae. Thus, the protruded discs and/or protruded bone spurs make the spinal cord canal narrow and produce symptoms of spinal cord compression.
Sometimes an asymptomatic condition of cervical stenosis can suddenly become symptomatic by trivial injury, due to the lack of reserve space around the spinal cord. Symptoms may include numbness of the arms or torso/legs, spastic weakness, clumsiness in walking or running, difficulty in balance, and disorders in bowel or bladder control. Treatment consists of conservative medical treatments or surgical treatments. Very early symptoms can be treated conservatively. However, surgical treatments may be necessary if symptoms of spinal cord compression become obvious.
Current conventional surgical treatments include: (1) anterior cervical discectomy or vertebrectomy followed by bone fusion and metal implant, and (2) posterior laminectomy or other similar posterior decompression procedures. Anterior procedures will eliminate compressing pathology more efficiently than posterior procedures. However, bone fusion will eliminate functioning motion in the neck. Posterior procedures are performed with or without bone fusion, but posterior laminectomy procedures do not actually eliminate the compressing pathology that is often located anterior to the spinal cord. Posterior procedures provide extra-room for the spinal cord posteriorly instead. Jho procedure accomplishes direct removal of compressing pathology while avoiding bone fusion in order to maintain neck motion.
A: 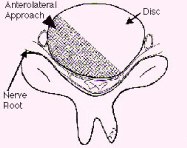 B:
B: 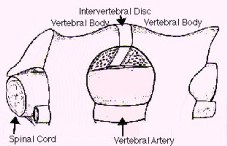
 B:
B: 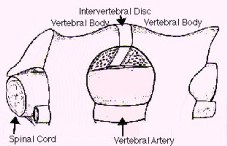
Figure 1: Schematic drawings, axial view (A) and lateral view (B), demonstrate decompression of the spinal cord through a small hole made at the side of the spine - the anterior microforaminotomy - while leaving the majority of the cervical disc and vertebral bone intact. Bone fusion is not necessary because the spine is stable. Neck motion is still preserved.
A:  B:
B:  C:
C:  D:
D: 
 B:
B:  C:
C:  D:
D: 
Figure 2: In a patient with severe spinal cord compression preoperatively at the C3-4, C4-5 and C5-6 levels (A, B), the Jho procedure for Cervical Stenosis sufficiently opens the spinal cord canal and the spinal cord is released from compression as seen in postoperative MR scans (C, D).
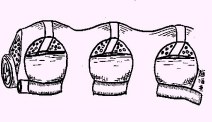
Figure 3: A schematic drawing demonstrates multilevel decompression via multiple foraminotomy holes made at the side of the spine.
A:  B:
B: 
 B:
B: 
Figure 4: MR scans, sagittal views, demonstrate cervical stenosis at C3-4, C4-5, C5-6 preoperatively (A) and subsequent excellent decompression of the spinal cord postoperatively (B) in another patient. In this technique, bone graft fusion is not necessary and not used. Thus, the neck motion is preserved.
A:  B:
B: 
 B:
B: 
Figure 5: A preoperative MR scan, axial view (A), reveals severe compression of the spinal cord by spondylotic bony spurs. A postoperative CT scan, axial view (B), shows the adequately widened spinal canal and decompressed spinal cord.
A:  B:
B: 
 B:
B: 
Figure 6: A postoperative 3D sagittal CT reconstruction depicts spinal canal decompression (A). Three foraminotomy holes (arrows) are demonstrated in this oblique reconstruction (B).
A:  B:
B: 
 B:
B: 
Figure 7: Intraoperative photographs show the spinal cord as seen through foraminotomy holes during surgical decompression of the spinal cord. Three foraminotomy holes are demonstrated (A), and a surgical instrument is passed between two foraminotomy holes to probe longitudinal decompression (B).
A:  B:
B:  C:
C: 
 B:
B:  C:
C: 
Figure 8. Flexion and extension dynamic X-rays show maintenance of motion and spinal stability (A,B). An AP X-ray show three foraminotomy holes and spinal stability (C).
Facts About the Jho Procedure for Cervical Stenosis
Discussion
Patients who have narrowed spinal cord canals in the neck region often suffer from numbness, weakness, pain in the arms, difficulty controlling urination, and difficulty with walking. Compared to conventional procedures which may not provide the surgeon access to the front portion of the canal (laminectomy techniques via a posterior approach) or those which may require excessive bone removal and fusion (anterior discectomy or vertebrectomy techniques), this new minimally invasive technique (Jho procedure) accomplishes efficient enlargement of the spinal cord canal and maintains the structural strength of the spinal column and neck motion. Through the use of small holes (called foraminotomy holes) made with the aid of an endoscope or an operating microscope, the procedure removes the calcium-bone buildup that is putting pressure on the spinal cord. An analogy that helps explain this procedure would be to picture removing some of the contents of a watermelon through a small hole without cutting the watermelon apart. Once the surgery is done, patients can usually go home the following day without collars or braces. Formal recovery at home usually occurs in the span of 4 to 6 weeks.
Definitions
foraminotomy - enlargement of an opening or passageway for a nerve.
stenosis - narrowing of a canal.
spondylotic - refers to spinal arthritis which is a non-inflammatory disease of the spine and can include excess bone growth.
References
Practice Manager: Robin A. Coret
Tel : (412) 359-6110
Fax : (412) 359-8339
Address : JHO Institute for Minimally Invasive Neurosurgery
Department of Neuroendoscopy
Sixth Floor, South Tower
Allegheny General Hospital
320 East North Avenue
Pittsburgh, PA 15212-4772
Copyright 2002-2032