Jho Institute for Minimally Invasive Neurosurgery Department of Neuroendoscopy
Spine Diseases
Brain Diseases
Trigeminal Neuralgia Surgery: Dr. Jho's Endoscopic Microvascular Decompression Surgery, Cranial Nerve Surgery
Dr. Jho's Minimally Invasive Cranial Nerve Surgery
Endoscopic Microvascular Decompression and Percutaneous Glycerol Rhizotomy
Professor & Chair, Department of Neuroendoscopy
Jho Institute for Minimally Invasive Neurosurgery
Having worked for approximately 20 years with Professor Jannetta (who pioneered the development of various Jannetta procedures for microvascular decompression), Dr. Jho has developed minimally invasive endoscopic microvascular decompression surgery for trigeminal neuralgia and other cranial nerve disorders. Microvascular decompression surgery was originally pioneered by Professor Jannetta, who has spent his entire neurosurgery career exploring various neurovascular compression syndromes.
Microvascular decompression (which consists of placement of small synthetic sponges between the compressing blood vessels and the affected cranial nerves) carries a good chance of relieving cranial nerve compression symptoms such as trigeminal neuralgia. For elderly or frail patients, percutaneous glycerol rhizotomy is a minimally invasive alternative treatment for trigeminal neuralgia. It consists of a drop or two of glycerol injected through the patient's cheek around the trigeminal nerve at the skull base using a spinal needle. This operation is performed under local anesthesia with sedation in the operating room and is done as outpatient surgery.
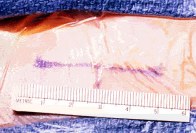
Figure 1. For microvascular decompression, a 4-cm skin incision is made behind the patient's ear. A small hole at the skull, retromastoid craniectomy, is made through this skin incision. This skull hole will be reconstructed at the end of the operation.
A: B:
B: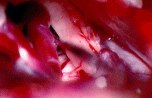 C:
C: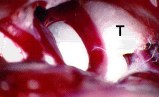
 B:
B: C:
C: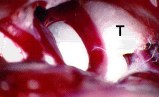
Figure 2. Intraoperative photographs show an arterial loop compressing the 5th cranial nerve (A; TN = trigeminal nerve), separation of the artery from the nerve (B), and placement of Teflon sponge (T) between the artery and the nerve (C).
A: 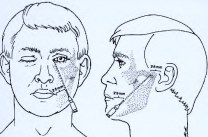 B:
B: 
 B:
B: 
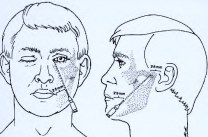
Figure 3. An artistic depiction shows needle placement during percutaneous glycerol rhizotomy (A). A fluoroscopic image taken during the procedure shows needle placement through the foramen ovale (B).
A:  B:
B: 
 B:
B: 
Figure 1. This intraoperative fluoroscopic image demonstrates appropriate glycerol placement (arrow) into the trigeminal cistern (A). A non-contrasted axial CT scan confirms placement of glycerol in the trigeminal cistern (arrow, B).
Overview
Trigeminal neuralgia is a symptom complex with severe facial pain. In classic trigeminal neuralgia, patients experience severe episodic lancinating (piercing) pain in the face. Although the attacks of pain can come in consecutive chains, each attack of pain may last only a few seconds. Touching, chewing, facial motion, and cold breezes are the usual triggers of facial pain attacks. Between attacks of pain, patients usually do not have any symptoms. In order to minimize the attacks of pain, patients often refrain from talking, facial expressive motion, or even eating. When patients have severe attacks, they can become easily dehydrated from avoiding beverages and food.
Although some patients with multiple sclerosis can develop trigeminal neuralgia due to demyelinating disease in the trigeminal nerve root, most patients with trigeminal neuralgia are classified as idiopathic due to the lack of any obvious cause. It was observed that most cases of idiopathic trigeminal neuralgia were caused by blood vessel compression at the trigeminal nerve root inside the head (neurovascular compression). In atypical form of trigeminal neuralgia, patients experience pain constantly or for an unusually prolonged period. This can be an extremely debilitating condition that reduces one's quality of life. Fortunately, the cases of trigeminal neuralgia that are caused by neurovascular compression may be effectively treated by surgical means.
Facts About These Surgeries
Discussion
Cranial nerve surgery is done through a small skull opening behind the ear and is referred to as retromastoid craniectomy. Skin incisions are usually two inches in length. When blood vessels cross and compress cranial nerves, various characteristic symptoms develop depending upon which cranial nerves are compressed. Trigeminal neuralgia develops by blood vessel compression of the trigeminal nerve, hemifacial spasm by compression of the facial nerve, intractable positional vertigo by compression of the vestibular nerve, tinnitus by compression of the cochlear nerve, glossopharyngeal neuralgia by compression on the glossopharyngeal nerve, and spasmodic torticollis by pressure on the spinal accessory nerve and upper cervical nerves.
Compressed cranial nerves are released from their compressing blood vessels under endoscopic visualization. Synthetic sponges are placed between the cranial nerve and blood vessels. Surgical openings are closed very cosmetically. Immediate surgical results of trigeminal neuralgia and hemifacial spasm are extremely satisfactory, with excellent outcomes in approximately 90 percent of the patients. Although trigeminal neuralgia has been known to recur on occasion, the recurrence of hemifacial spasm is rare.
Reference
Practice Manager: Robin A. Coret
Tel : (412) 359-6110
Fax : (412) 359-8339
Address : JHO Institute for Minimally Invasive Neurosurgery
Department of Neuroendoscopy
Sixth Floor, South Tower
Allegheny General Hospital
320 East North Avenue
Pittsburgh, PA 15212-4772
Copyright 2002-2032