Jho Institute for Minimally Invasive Neurosurgery Department of Neuroendoscopy
Spine Diseases
Brain Diseases
Aneurysm Surgery, Cerebral Aneurysm Surgery: Dr. Jho's Mini-craniotomy Brain Aneurysm Surgery
Dr. Jho's "Band-Aid" Eyebrow Incision Skull Base Surgery for Cerebral Aneurysms
Professor & Chair, Department of Neuroendoscopy
Jho Institute for Minimally Invasive Neurosurgery
"Band-Aid" skull base brain surgery for cerebral aneurysms has been developed for minimally invasive cerebral aneurysm surgery. The small surgical skin incision follows the contour of the eyebrow. A tiny skull opening is made for exposure at the skull base where the cerebral aneurysm is located. After a surgical aneurysm clip is successfully placed at the neck of the aneurysm sac, the surgical opening is closed cosmetically. Metallic brain retractors are not used during surgery in order to avoid unwanted brain damage.
A:  B:
B:  C:
C: 
 B:
B: 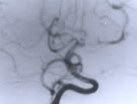 C:
C: 
Figure 1. A preoperative cerebral arteriogram (A) shows a basilar tip aneurysm. A postoperative arteriogram, after aneurysm clipping via a superolateral orbital craniotomy, confirms successful clipping (B). A patient with a healed superolateral orbital craniotomy incision line (C) (arrows).
Facts About This Surgery
Discussion
Utilizing a small hole in the skull above and to the side of the eyebrow, this minimally invasive skull base procedure provides a direct "shortcut" approach to tumors and aneurysms. Nicknamed "Band-Aid" surgery because only a "Band-Aid" type of small bandage is needed to cover the postoperative incision, this surgery does not sacrifice exposure for the surgeon while providing the many benefits of being less invasive. Cerebral aneurysms can be reached through a two-inch skin incision and a small bone hole called a craniotomy. This technique is referred to as a superolateral craniotomy because the approach is above the eye and slightly to the side. Brain retractors are not used, which reduces the risk of brain injury. Positive feedback has been received concerning the cosmetic healing of the small incision.
Reference
Practice Manager: Robin A. Coret
Tel : (412) 359-6110
Fax : (412) 359-8339
Address : JHO Institute for Minimally Invasive Neurosurgery
Department of Neuroendoscopy
Sixth Floor, South Tower
Allegheny General Hospital
320 East North Avenue
Pittsburgh, PA 15212-4772
Copyright 2002-2032