Jho Institute for Minimally Invasive Neurosurgery Department of Neuroendoscopy
Spine Diseases
Brain Diseases
Cervical Stenosis surgery without bone fusion: Dr. Jho's Spinal Cord Decompression via Anterior Foraminotomy for Spondylotic Cervical Stenosis or OPPL
Dr. Jho's Minimally Invasive Cervical Stenosis Surgery (The Jho procedure for cervical stenosis): Spinal Cord Decompression via Anterior Foraminotomy for Spondylotic Cervical Stenosis, or Ossified Posterior Longitudinal Ligament (OPPL)
Professor & Chair, Department of Neuroendoscopy
Jho Institute for Minimally Invasive Neurosurgery
Current conventional surgery for cervical stenosis includes anterior discectomy or vertebrectomy followed by bone fusion and metal plate implantation, or posterior laminectomy. Bone fusion surgery will prolong surgical recovery and once healed, the neck motion will be restricted. Posterior laminectomy usually does not address compressing pathology effectively because the compressing pathology, often bone spurs, is usually located anterior to the spinal cord. Posterior laminectomy simply provides an extra room behind the spinal cord.
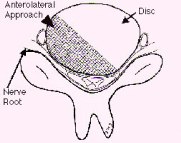
In order to accomplish minimally invasive, efficient elimination of the compressive pathology to the spinal cord and to maintain the motion segment, the Jho procedure for Cervical Stenosis Surgery was developed. The compressing pathology is removed via a small microforaminotomy hole or holes made at the side of the cervical spine via a small incision made at the anterior neck (Figure 1). This operation does not require bone fusion or metal plate-screw implantation. Postsurgical discomfort is relatively minimal. Wearing postoperative brace is not necessary. Hospital stay is average overnight.
A: 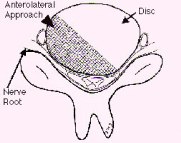 B:
B: 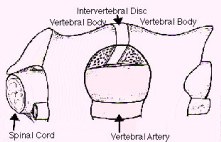
 B:
B: 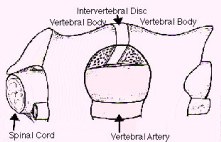
Figure 1: Schematic drawings, axial view (A) and lateral view (B), demonstrate decompression of the spinal cord through a small hole made at the side of the spine - the anterior microforaminotomy - while leaving the majority of the cervical disc and vertebral bone intact. Bone fusion is not necessary because the spine is stable. Neck motion is still preserved.
Cervical stenosis is a disease condition that narrows the spinal cord canal in the cervical spine and causes symptoms of spinal cord compression. Although similar to Cervical Disc Herniation in many ways, Cervical Stenosis involves a narrowing of the spinal canal that chokes the spinal cord rather than a focal protrusion of disc material that compresses a part of the spinal cord and/or nerve roots.
Cervical stenosis can be categorized into two different types: a congenital form and an acquired form. Although various congenital conditions may cause the narrowing of the spinal cord canal, it is also possible for normal people to have a relatively narrow spinal cord canal at birth. The acquired form of cervical stenosis is generally developed by wear-and-tear. In Cervical Stenosis, the intervertebral discs are protruded and bony spurs are built-up all along the edges of the vertebrae. Thus, the protruded discs and/or protruded bone spurs make the spinal cord canal narrow and produce symptoms of spinal cord compression.
Sometimes an asymptomatic condition of cervical stenosis can suddenly become symptomatic by trivial injury, due to the lack of reserve space around the spinal cord. Symptoms may include numbness of the arms or torso/legs, spastic weakness, clumsiness in walking or running, difficulty in balance, and disorders in bowel or bladder control. Treatment consists of conservative medical treatments or surgical treatments. Very early symptoms can be treated conservatively. However, surgical treatments may be necessary if symptoms of spinal cord compression become obvious.
Current conventional surgical treatments include: (1) anterior cervical discectomy or vertebrectomy followed by bone fusion and metal implant, and (2) posterior laminectomy or other similar posterior decompression procedures. Anterior procedures will eliminate compressing pathology more efficiently than posterior procedures. However, bone fusion will eliminate functioning motion in the neck. Posterior procedures are performed with or without bone fusion, but posterior laminectomy procedures do not actually eliminate the compressing pathology that is often located anterior to the spinal cord. Posterior procedures provide extra-room for the spinal cord posteriorly instead. Jho procedure accomplishes direct removal of compressing pathology while avoiding bone fusion in order to maintain neck motion.
A:  B:
B:  C:
C:  D:
D: 
 B:
B:  C:
C:  D:
D: 
Figure 2: In a patient with severe spinal cord compression preoperatively at the C3-4, C4-5 and C5-6 levels (A, B), the Jho procedure for Cervical Stenosis sufficiently opens the spinal cord canal and the spinal cord is released from compression as seen in postoperative MR scans (C, D).
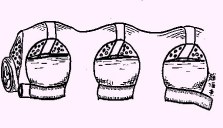
Figure 3: A schematic drawing demonstrates multilevel decompression via multiple foraminotomy holes made at the side of the spine.
A:  B:
B: 
 B:
B: 
Figure 4: MR scans, sagittal views, demonstrate cervical stenosis at C3-4, C4-5, C5-6 preoperatively (A) and subsequent excellent decompression of the spinal cord postoperatively (B) in another patient. In this technique, bone graft fusion is not necessary and not used. Thus, the neck motion is preserved.
A:  B:
B: 
 B:
B: 
Figure 5: A preoperative MR scan, axial view (A), reveals severe compression of the spinal cord by spondylotic bony spurs. A postoperative CT scan, axial view (B), shows the adequately widened spinal canal and decompressed spinal cord.
A:  B:
B: 
 B:
B: 
Figure 6: A postoperative 3D sagittal CT reconstruction depicts spinal canal decompression (A). Three foraminotomy holes (arrows) are demonstrated in this oblique reconstruction (B).
A:  B:
B: 
 B:
B: 
Figure 7: Intraoperative photographs show the spinal cord as seen through foraminotomy holes during surgical decompression of the spinal cord. Three foraminotomy holes are demonstrated (A), and a surgical instrument is passed between two foraminotomy holes to probe longitudinal decompression (B).
A:  B:
B:  C:
C: 
 B:
B:  C:
C: 
Figure 8. Flexion and extension dynamic X-rays show maintenance of motion and spinal stability (A,B). An AP X-ray show three foraminotomy holes and spinal stability (C).
Facts About the Jho Procedure for Cervical Stenosis
Discussion
Patients who have narrowed spinal cord canals in the neck region often suffer from numbness, weakness, pain in the arms, difficulty controlling urination, and difficulty with walking. Compared to conventional procedures which may not provide the surgeon access to the front portion of the canal (laminectomy techniques via a posterior approach) or those which may require excessive bone removal and fusion (anterior discectomy or vertebrectomy techniques), this new minimally invasive technique (Jho procedure) accomplishes efficient enlargement of the spinal cord canal and maintains the structural strength of the spinal column and neck motion. Through the use of small holes (called foraminotomy holes) made with the aid of an endoscope or an operating microscope, the procedure removes the calcium-bone buildup that is putting pressure on the spinal cord. An analogy that helps explain this procedure would be to picture removing some of the contents of a watermelon through a small hole without cutting the watermelon apart. Once the surgery is done, patients can usually go home the following day without collars or braces. Formal recovery at home usually occurs in the span of 4 to 6 weeks.
Definitions
foraminotomy - enlargement of an opening or passageway for a nerve.
stenosis - narrowing of a canal.
spondylotic - refers to spinal arthritis which is a non-inflammatory disease of the spine and can include excess bone growth.
References
Practice Manager: Robin A. Coret
Tel : (412) 359-6110
Fax : (412) 359-8339
Address : JHO Institute for Minimally Invasive Neurosurgery
Department of Neuroendoscopy
Sixth Floor, South Tower
Allegheny General Hospital
320 East North Avenue
Pittsburgh, PA 15212-4772
Copyright 2002-2032